DISEASES
Immune-mediated Hemolytic Anemia in Dogs - Symptoms and Treatment
페이지 정보
본문


What is autoimmune hemolytic anemia (AIHA) in dogs?
Hemolytic anemia is a condition of the immune system that targets and destroys its own red blood cells in the bloodstream. Red blood cells are created in the bone marrow and circulate through the blood vessels to supply oxygen and nutrients to the body. As part of this process, damaged or aging red blood cells are removed from circulation and replaced with fresh ones.
Hemolytic anemia is an autoimmune disease where the immune system mistakenly attacks and destroys red blood cells, leading to a shortage that the bone marrow cannot keep up with. This rapid decrease in red blood cell count leads to lowered oxygen levels in the blood and ultimately results in anemia.
Hemolytic anemia can be caused by immune system disorders or the production of antibodies that attack red blood cells, as well as other illnesses or exposure to toxins.
Causes of canine hemolytic anemia
Hemolytic anemia is a disease of the immune system that attacks and destroys red blood cells. In this disease, healthy red blood cells are recognized as damaged red blood cells and promptly destroyed.
Primary causes
Most cases of hemolytic anemia in dogs are caused by:
- Abnormalities in the autoimmune system
- Production of antibodies that attack normal red blood cells
Secondary causes
When red blood cells are altered by other diseases or infections, a dog's immune system recognizes them as infiltrators that should be wiped out.
- Infection by Ehrlichia, leptospira, etc.
- Blood parasites such as babesia
- Reaction to medication
- Venom from an animal
- Toxicosis or poisoning (ex. Allium poisoning from ingesting onion or garlic)
- Bee sting
- Tumor
Symptoms of hemolytic anemia in dogs
If your dog has hemolytic anemia, you may notice symptoms of severe anemia as well as any of the following symptoms:
- Pale gums
- Lethargy
- Exercise intolerance
- Fainting
- Dizziness
- Shortness of breath or rapid breathing
- Disorientation
- Yellowing of mucous membranes (due to hyperbilirubinemia)
- Loss of appetite
- Vomiting
- Change in urine color (due to hyperbilirubinemia)
The risk and when to see a vet for canine hemolytic anemia
If symptoms such as hemorrhaging round spots on the surface of your dog’s skin occur while suspecting immune-mediate hemolytic anemia, the prognosis may be poor. It is known that hemolytic anemia is accompanied by hyperbilirubinemia, thrombocytopenia, leukocytosis, azotemia, and hypoalbuminemia.
Breeds more susceptible to hemolytic anemia include:
- Vizslas
- Irish Setters
- Cocker Spaniels
- Scottish Terriers
- Old English Sheepdogs
- Miniature Schnauzers
- English Springer Spaniels
- Poodles
- Dobermans
- Dachshunds
How to deal with hemolytic anemia in dogs at home
If you suspect your dog has ingested any foreign substance that can cause poisoning symptoms, it is essential to induce vomiting as soon as possible. If that is not possible to do so at home, visiting a veterinarian hospital and seeking professional treatment is required.
In the case, of a dog exhibiting any anemia-related symptoms, visit a veterinary hospital as soon as possible and get tested. Dogs with hemolytic anemia require regular blood tests and symptom monitoring for the best prognosis.
Diagnosing autoimmune hemolytic anemia in dogs

If you suspect your pet is suffering from AIHA and visit a vet, you can expect your veterinarian to first conduct an interview to gather as much relevant information on your pet’s symptoms. This will be followed by a physical examination and additional tests to accurately diagnose the condition.
-
CBC test
CBC can determine the number and percentage (PCV) of red blood cells. The normal level of PCV in dogs is 35-55%, and anemia is diagnosed when it is less than 35%.
-
Blood smear test
The collected blood is smeared, and the shape and size of red blood cells are evaluated under a microscope.
-
Serology tests and more
Once symptoms of anemia are confirmed, tests such as a serological, antibody, blood PCR, Coombs, or reticulocyte count tests can be conducted to differentiate between primary and secondary causes. If a secondary cause is suspected, additional serum, urine, chest and abdominal radiographs, and ultrasound tests can be performed.
Treatment for hemolytic anemia in dogs
Usually, in the early stages, patients are hospitalized in intensive care with fluid therapy.
-
Blood transfusion
Severe anemia may require a blood transfusion, and a blood sample is taken to determine the blood type. A blood transfusion may be performed initially while various tests are conducted to determine the cause of hemolytic anemia. The primary objective of a blood transfusion is to identify the underlying cause and stabilize it until other therapeutic measures take effect.
-
Immunosuppressive therapy
If hemolytic anemia is determined to be caused by a primary cause, specifically autoimmune system abnormalities, immunosuppressive therapy will be administered. The primary immunosuppressive drugs used are corticosteroids such as prednisolone. Depending on the condition, cyclosporine may be utilized, or other medications like leflunomide, mycophenolate mofetil, or azathioprine may be prescribed to minimize steroid reliance.
-
Blood clot prevention
Anticoagulant therapy may be administered to prevent blood from clotting.
-
Plasmapheresis
In a recent paper, it was confirmed that plasmapheresis effectively removes attacking antibodies and inhibits aggregation.
-
Splenectomy
Hemolytic anemia is a condition that involves the destruction of red blood cells. Splenectomy, a commonly used treatment in humans, removes the spleen, which plays a role in destroying damaged red blood cells. By slowing down the destruction process, ablation can help manage the condition. This treatment is typically only considered when traditional therapies have failed and after an ultrasound has identified an issue with the spleen.
If it is confirmed that hemolytic anemia is caused by a secondary cause, the following treatments for the underlying cause are performed.
-
Parasites
If a blood parasite, such as babesia, is the cause, it can be treated with antibiotics, focusing on treating the infection.
-
Venom
If caused by a toxin such as a snake venom, appropriate treatment such as dialysis or fluid therapy is required.
-
Toxicosis
If caused by onion or garlic ingestion, vomiting may be administered if it is not long after the ingestion.
Prevention of hemolytic anemia in dogs
Regular blood tests and symptom monitoring are necessary to prevent anemia. During the stabilization phase of hemolytic anemia, the dose of immunosuppressants is reduced to minimize side effects. Due to the high likelihood of recurrence, the condition must be closely monitored when reducing the drug's dose to prevent relapse. It is recommended to pay close attention to secondary causes of anemia such as parasites and toxins. Keeping your pet up to date on preventives and keeping a clean environment can help reduce the chances of anemia.
Find out more about your dog’s symptoms and diseases on the Buddydoc app!
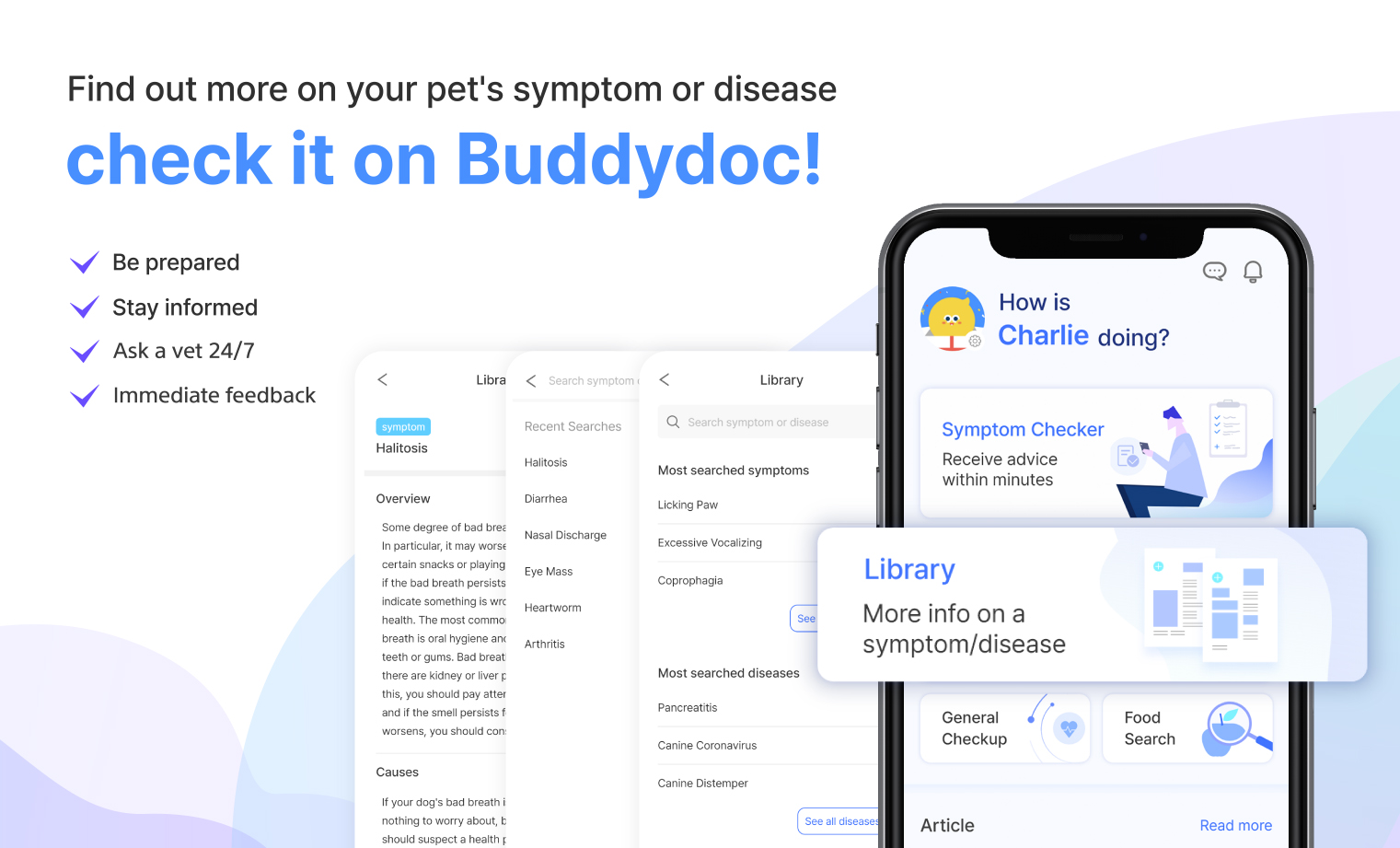
The Buddydoc library is filled with everything you’d want to know about each symptom and disease your pet may experience. If you would like to find out more about the causes, signs, treatments, preventions, and more for your dog’s disease. Try out the Buddydoc app and search for your pet’s symptoms or diseases in the Buddydoc library.












