DISEASES
Lymphangiectasia in Dogs - Expectancy, Symptoms, and Treatment
페이지 정보
본문


What is canine lymphangiectasia?
Intestinal lymphangiectasia is a condition in which the absorption of proteins is impaired due to the dilation of lymphatic vessels. In the lymphatic system, its primary role is to transport waste products from tissues into the bloodstream, absorb digested fats in the intestine, and provide immune activity in various parts of the dog’s body. As a result of lymphangiectasia, fats or proteins leak into the intestinal tract.
Diseases in which protein is excreted through the intestine without being absorbed are collectively referred to as Protein-Losing Enteropathy (PLE). Lymphangiectasia can be caused by either congenital abnormal lymphatic vessels or obstruction of lymphatic flow due to increased venous pressure due to inflammation or congestive heart failure. Pets with Lymphangiectasia typically experience symptoms such as weight loss, chronic diarrhea, and vomiting. A diagnosis is made through a blood test or biopsy and a treatment plan tailored to the underlying cause is established. Dietary management plans are also created to provide proper nutrition to help counter the effects of the leakage.
Causes of intestinal lymphangiectasia in dogs
The exact cause of this phenomenon is still not fully understood. Certain bowel diseases may also accompany lymphangiectasia, however, the exact relationship between the two remains unclear as well.
Possible causes of lymphangiectasia are:
-
Inflammatory bowel disease (IBD)
Inflammation of the intestines caused by food allergies, parasites, bacteria, viruses, or genetics can result in lymphangiectasia.
-
Venous hypertension
Conditions that increase blood pressure in veins, such as congestive heart failure or portal hypertension, can lead to lymphangiectasia.
-
Blockage of the thoracic duct
The thoracic duct is a type of lymphatic vessel that connects to a vein. Blockage of the thoracic duct by something such as a tumor can result in lymphangiectasia.
-
Cancers that originate in the intestines, such as lymphoma
-
Breed predisposition
Breeds such as Basenji, Norwegian Lundshund, Irish Soft-Coated Wheaten Terrier, Yorkshire Terrier, German Shepherd, Rottweiler, and Chinese Shar-Peis are on a list of dogs that are known to have congenital heart issues.
Symptoms of lymphangiectasia in dogs
The primary symptoms of lymphangiectasia are weight loss, diarrhea, and vomiting. However, the symptoms may be vague and occur sporadically. In some cases, the symptoms may not even be noticeable and can only be detected during a routine health checkup.
The following are all the symptoms associated with canine lymphangiectasia:
- Weight loss
- Anorexia/Loss of appetite
- Diarrhea
- Vomiting
- Abdominal swelling
- Abdominal pain
- Coughing/Difficulty breathing
- Swollen limbs
Risk of canine lymphangiectasia and when you should see a vet
The symptoms of lymphangiectasia are often non-specific and can be caused by other diseases, making it hard to distinguish without a routine veterinary checkup. If your dog is experiencing persistent weight loss or chronic diarrhea and vomiting, it is crucial to take them to a veterinarian for an examination. Additionally, if you notice your dog's abdomen appearing swollen or full of fluid when touched or if they are exhibiting signs of abdominal pain, it is imperative to contact your veterinarian for an examination.
How to deal with intestinal lymphangiectasia in dogs at home
If your pet is experiencing temporary and mild symptoms of lymphangiectasia, transitioning their diet to a more easily absorbed option, such as a nutritionally balanced or hydrolyzed protein diet, may help. It may take anywhere from one week to twelve weeks to see a response to this dietary change. Additionally, supplementing their diet with probiotics can alleviate symptoms.
Diagnosing canine lymphangiectasia

Diagnosing lymphangiectasia can be challenging as its symptoms are often nonspecific, requiring tests to differentiate from other diseases that present with similar symptoms.
Questions your veterinarian may ask for a diagnosis of lymphangiectasia include:
- Does your dog have symptoms such as diarrhea, vomiting, or weight loss?
- When did the symptoms appear, how often, and how long did they last?
- Has your dog lost weight suddenly?
- Have you noticed any recent changes in your dog’s appetite or energy?
- Tell us about your dog’s diet and snacks.
- Has your dog taken any repellents recently?
- Does your dog currently have any other medical conditions?
Based on the answers to this question, the veterinarian will select the necessary tests for diagnosis. The list of tests varies and may require endoscopy or tissue biopsy to confirm the diagnosis.
-
CBC test
A CBC test checks for the increase or decrease of inflammatory cells and can also determine if there has been any bleeding in the intestine.
-
Blood chemistry test
A blood chemistry test can detect protein loss. Low levels of albumin, cholesterol, and calcium are often seen in patients with lymphangiectasia. However, a decrease in albumin can also be caused by diseases in other organs, such as the kidneys, liver, and adrenal glands. The veterinarian will consider symptoms present in the patient and results from tests such as urinalysis, X-rays, and an abdominal ultrasound to make an accurate diagnosis.
-
Fecal exam
A stool test can check for bacterial or parasitic infections.
-
Blood vitamin B12 concentration test
A vitamin B12 concentration test for cobalamin can determine if the ability to absorb nutrients from the intestine is reduced.
-
Blood folic acid level test
A folate level test can help determine if there is an imbalance of the normal flora in a dog’s gut.
-
Blood clotting test
Because blood clotting factors are often lost in the presence of lymphangiectasia, blood clotting tests can be performed before a biopsy or when persistent bleeding is suspected.
-
X-ray
X-rays of the abdomen are used to view the organs in the abdominal cavity as a whole. It can also check for fluid buildup and tumors. Additionally, a chest radiograph can check for abnormalities in the heart or lungs.
-
Abdominal ultrasound
The thickness and degree of inflammation of the intestinal wall or mucosal layer, inflammation of the peritoneum, presence or absence of tumors, and abnormalities in the kidneys or liver can all be evaluated through ultrasound.
-
Endoscopy
The stomach can be examined through the oral cavity. Abnormalities in the intestine can be assessed by accessing the large intestine through the anus. If there is a suspicion of lymphangiectasia, dilated lymphatic vessels may be more easily visualized by feeding a high-fat diet, such as edible oil or cream, before endoscopy.
-
Tissue biopsy
A tissue biopsy is typically performed to confirm the diagnosis. If access through an endoscope is challenging, a biopsy may be conducted through surgical intervention after administering anesthesia.
Treatment for canine lymphangiectasia
The treatment process for intestinal lymphangiectasia depends on the underlying cause and the overall health of the dog. It can be challenging, and it may take a considerable amount of time, and in some cases, a cure may not be possible. The ultimate goal of treatment for lymphangiectasia is to raise the lowered albumin level and alleviate symptoms associated with lymphangiectasia.
-
Drainage
If your dog has a significant amount of pleural effusion or fluid buildup, they may require immediate drainage using a needle and syringe. In cases of severe electrolyte imbalance or malnutrition, fluid treatment or a nutrient supply may be necessary. Additionally, if there is a suspicion of thromboembolism or a likelihood of it occurring, medication may be necessary to prevent and treat it.
-
Diet
Nutritional management plays a crucial role in the care of dogs with lymphangiectasia. To support their well-being, we often prescribe a customized diet that is easy to digest, rich in protein, and low in fat. In some cases, we may recommend using hydrolyzed protein or switching to a new source of protein altogether. Additionally, vitamin deficiencies are common in these patients, so vitamin supplements may be necessary. For severe symptoms, it is advisable to consult with a veterinarian specializing in nutrition.
-
Medication
If a pet is diagnosed with both inflammatory bowel disease (IBD) and lymphangiectasia, the veterinarian may prescribe steroids and immunosuppressive drugs to suppress the immune response. Antibiotics may also be prescribed to correct intestinal dysbiosis. If thromboembolism is suspected, antithrombotic agents may be prescribed, and if fluid buildup continues to accumulate, diuretics may be prescribed.
-
Probiotics
Probiotics like lactobacillus may be prescribed to help balance the normal flora in the intestine.
Prevention of lymphangiectasia in dogs
Because the cause of lymphangiectasia is still unknown, it is a difficult disease to prevent. It may be caused by various factors and its symptoms are often vague. To accurately diagnose the condition and prevent it from worsening, pet owners should closely observe their dog for symptoms such as continuous weight loss and repeated diarrhea and seek an examination at a veterinary hospital.
Find out more about your dog’s symptoms and diseases on the Buddydoc app!
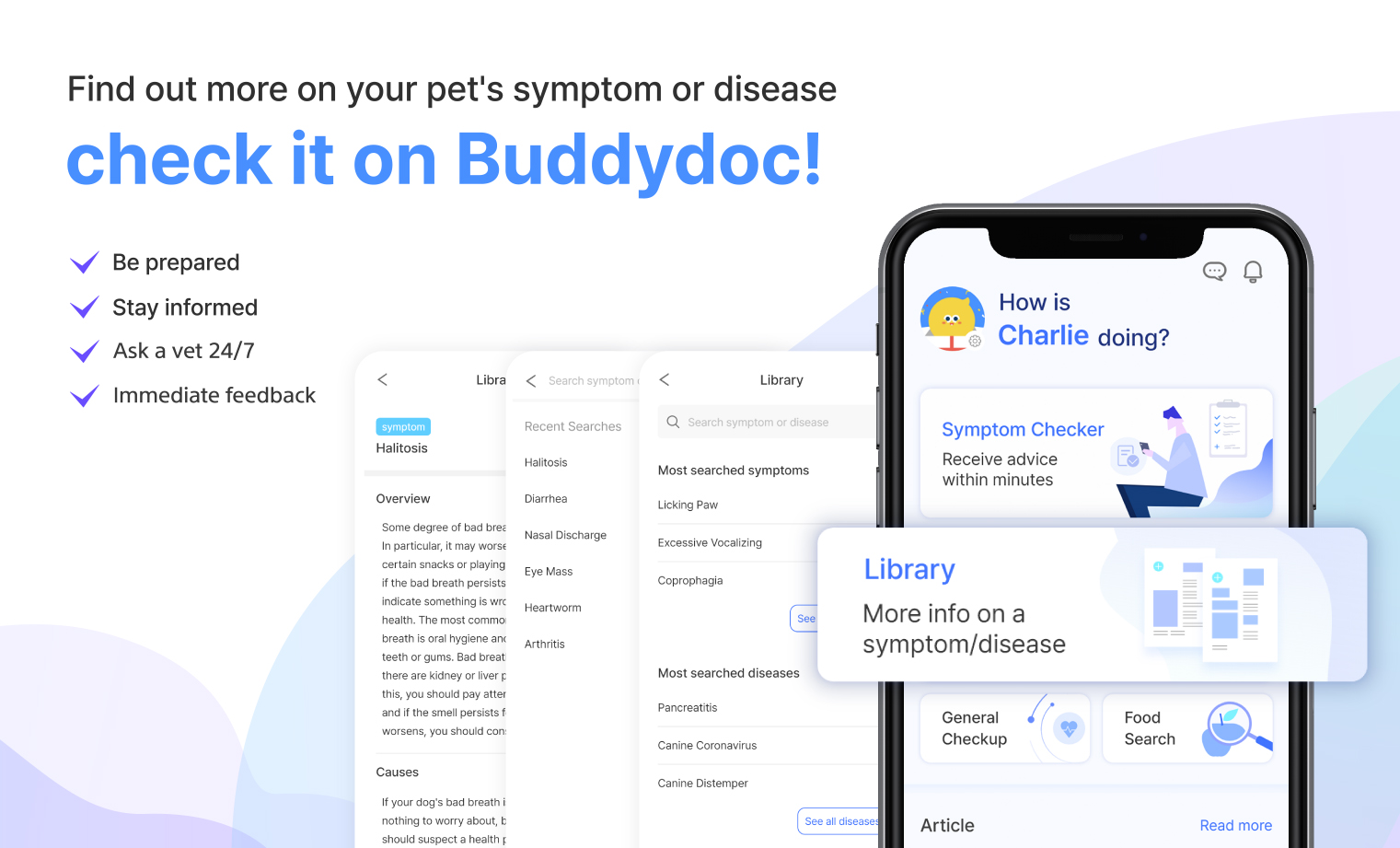
The Buddydoc library is filled with everything you’d want to know about each symptom and disease your pet may experience. If you would like to find out more about the causes, signs, treatments, preventions, and more for your dog’s disease. Try out the Buddydoc app and search your pet’s symptoms or diseases in the Buddydoc library.












